Cancer, Diet and Lifestyle
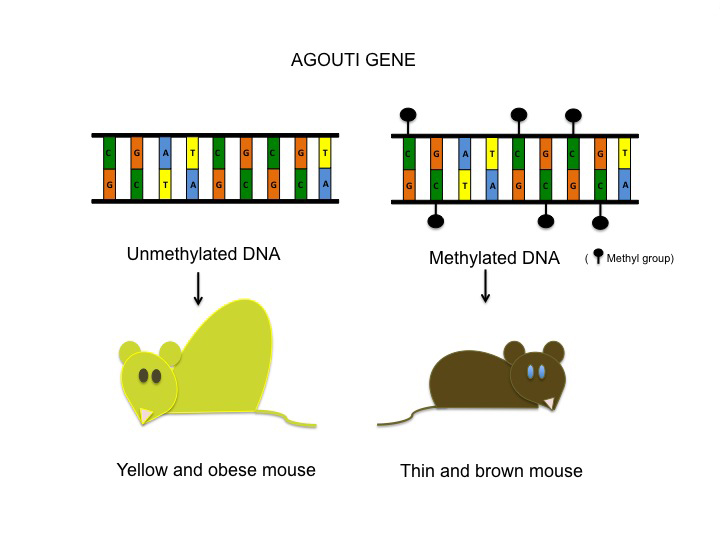
Lifestyles can interact with the epigenome, defined as the network of compounds around our genes that are capable of altering gene expression in response to environmental influences. The ultimate action can result in cancer prevention.
DIET MODIFICATIONS
The general risk factors of cancer include obesity, physical inactivity, alcohol consumption and/or poor nutrition. These factors have the potential to determine if a cancer will result or in the opposite case, be suppressed.
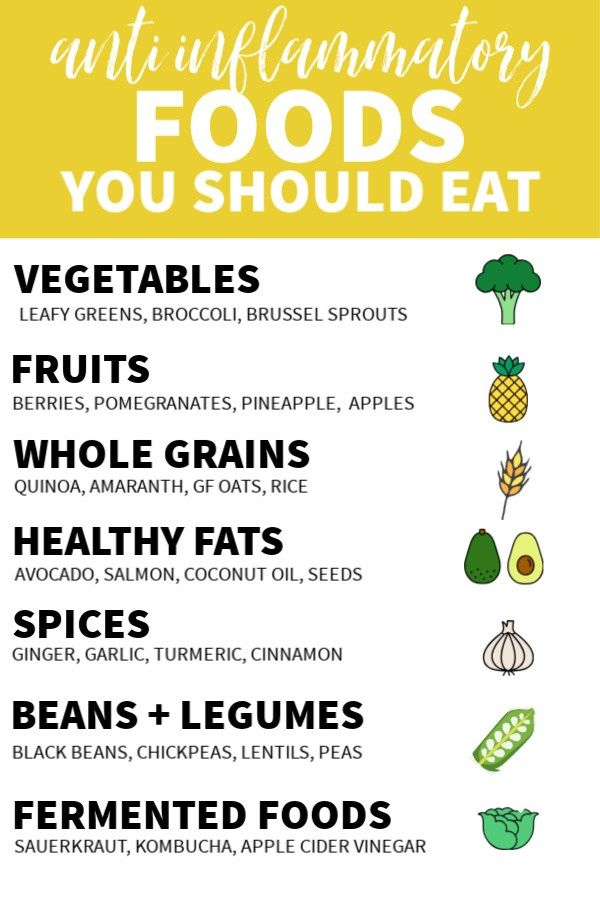
Consume a nutrient dense, whole-foods diet that predominantly includes plant foods. As Michael Pollan puts it, “Eat food, not too much, mostly plants.” Plant foods are rich in nutrients and phytochemicals that work synergistically to prevent many chronic diseases, primarily heart disease and cancer. Evidence exists that up to 45% of colon cancer cases could be avoided through diet and lifestyle changes alone.
Limit your consumption of high-calorie foods, primarily in the form of ultra-processed foods that are major contributors to weight gain leading to type 2 diabetes, or insulin resistance.
Cancers of the liver, pancreas, endometrium, colon, rectum, breast, and bladder are at higher risks for developing in obesity. Being overweight also raises the risk of developing non-Hodgkin’s lymphoma, multiple myeloma and gallbladder, liver, cervical, ovarian, and aggressive prostate cancers.
Be as lean as possible without becoming underweight. It may be helpful to be able to calculate your own weight status by using the Body Mass Index (BMI).
You simply divide your weight in pounds by your height in inches squared X 703.
For example: BMI =140 pounds divided by 64 inches squared (4096) X 703 = 24.0. A healthy BMI is 20 – 24. Being underweight is considered a BMI of less than 19.0.
Limit your consumption of red meat (including beef, pork and lamb). There are several reasons:
The International Agency for Research on Cancer (IARC) classifies red meat as a “probably carcinogen”. You don’t need to give up meat; however, an intake of up to 18 ounces a week can be safely consumed without too much concern. BTW, 4 oz. is about the size of a deck of cards.
Another factor that raises cancer risk is the overcooking of red meat that produces charred areas of the meat – goodbye grill marks?). These create carcinogenic heterocyclic amines (HCAs) that have been linked to pancreatic and colon cancers.
Another carcinogenic compound comes from burning the fat from meat when grilling that produce polycyclic aromatic hydrocarbons (PAHs), linked to stomach cancer.
Hint: Both compounds can be lessened by using a marinade on the meat.
Highly processed meats such as bacon, hot dogs, and lunch meats are known for their nitrite and nitrate content used as preservatives. Smoking meats can lead to the formation of N-nitroso compounds which are considered carcinogenic.
Avoid deep-fried foods. When cooked in this manner, foods are exposed to a chemical called acrylamide that increases the risk of prostate cancer.
There are other lifestyle factors that can influence epigenetically the risk of any chronic disease. Alcohol intake, for example is important due to the carcinogenic effects of alcohol itself.
“Chronic inflammation, which is strongly associated with being overweight, can increase the risk of developing cancer. Excess belly fat produces hormones that can raise levels of insulin, estrogen and leptin, all of which have been linked to cancer development.” (Finlayson, 2019).
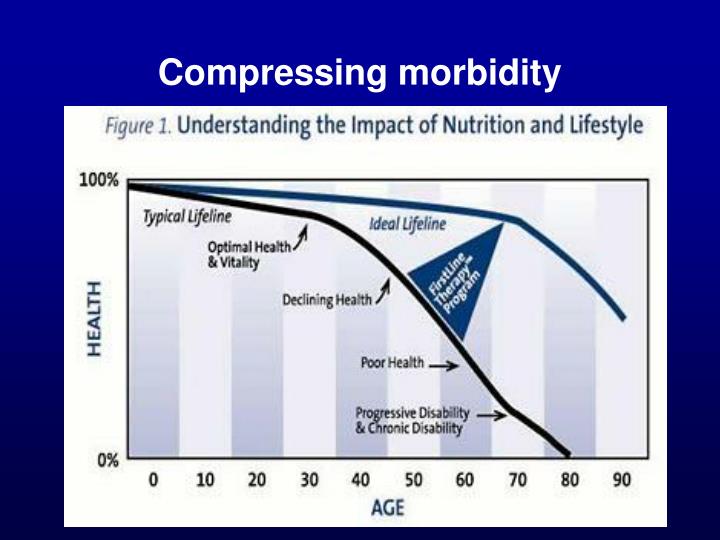
The interconnected factors that trigger chronic diseases are vast and subject to manipulation by the body as well as our microbial environment. It would be wise to attempt to take the best care of your body as you possibly can and begin at an early age. Aging as you know itself becomes a central factor in the development of any chronic disease. In 1980, Dr. James Fries, Professor of Medicine, Stanford University introduced the compression of morbidity theory. This theory states that “most illness was chronic and occurred in later life and postulated that the lifetime burden of illness could be reduced if the onset of chronic illness could be postponed and if this postponement could be greater than increases in life expectancy.” That theory tells it all. (Unknown source). SJF
Source: Judith Finlayson. You Are What Your Grandparents Ate: What You Need to Know About Nutrition, Experience, Epigenetics & the Origins of Chronic Disease, 2019